
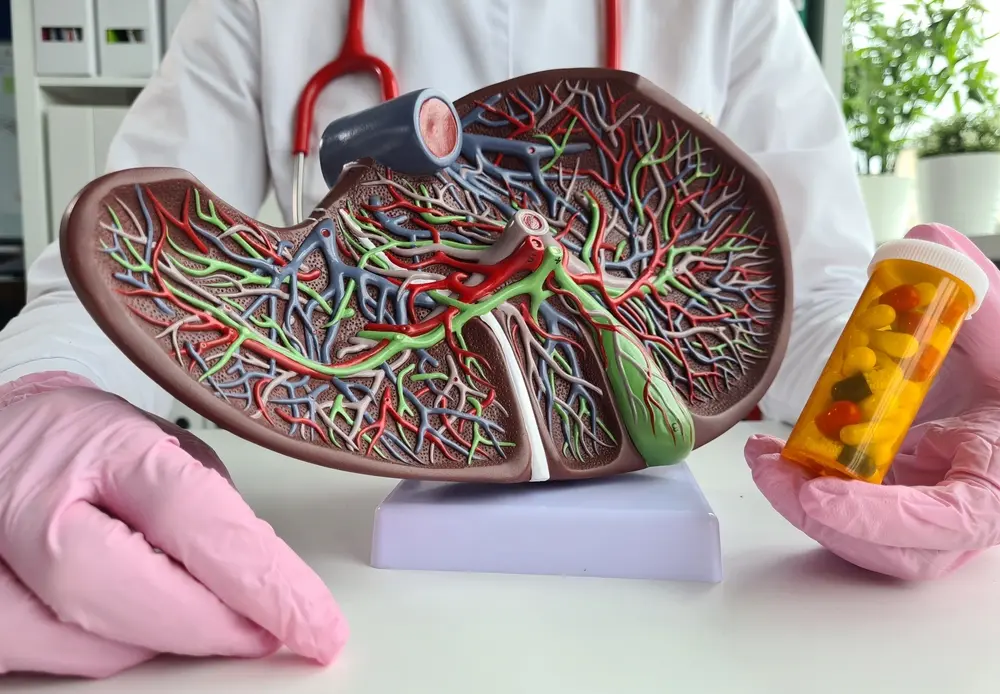
The bile ducts in the liver are lined by special cells called cholangiocytes. These cells help produce, adjust, and move bile—a digestive fluid—from the liver to the intestines. When cholangiocytes don’t work correctly, it can cause long-term bile duct diseases called cholangiopathies, which are severe and can become disabling.
Two major types of these bile duct diseases are Primary Biliary Cholangitis (PBC) and Primary Sclerosing Cholangitis (PSC). Both are thought to be caused by the immune system mistakenly attacking bile ducts, although the exact causes are still unknown. Here’s a simple breakdown:
Both these autoimmune liver diseases involve inflammation and scarring, which can eventually cause liver failure. Right now, there’s no cure for PBC or PSC. Treatments exist but mainly aim to slow disease progression and manage symptoms.
For PBC, medications can sometimes help, but they don’t work for everyone. With PSC, the options are even more limited. Most patients are only able to manage symptoms and hope their disease doesn’t worsen too quickly. In severe cases, patients often need a liver transplant. This is why clinical trials are essential for people with PBC and PSC.

Clinical studies test the efficacy and safety of new therapies that could improve liver health, reduce symptoms, and potentially halt or even reverse some of the liver damage caused by these diseases. Such trials bring real hope that people with PBC and PSC might have access to treatments that could change the course of these conditions. The latest PSC research aims to:
Clinical trials progresses through phases to ensure new treatments are safe and effective. Knowing these phases can help you understand the process and what to expect if you decide to participate:
Phase 1: The first step tests whether a new drug is safe, often with a small group of people. Researchers look for any side effects and try to find the proper dosage.
Phase 2: This phase expands to test how well the treatment works, still monitoring safety but with a larger group of participants.
Phase 3: Now, the treatment is tested on a much larger scale, often compared to standard treatments. This phase confirms its effectiveness and checks for any rare side effects.
Phase 4: After approval, these studies continue to monitor the long-term safety and effectiveness of the treatment.
Each phase helps researchers confirm that a treatment is both safe and effective before it becomes available to the broader public.
Eligibility criteria for clinical trials vary depending on the study. Researchers typically look for specific characteristics to ensure the trial results are accurate and meaningful. You may be eligible if you:
Your doctor can help you determine whether a specific trial might be a good fit and whether the potential benefits align with your health needs.
For many people, clinical trials can offer a unique opportunity to explore treatments that aren’t yet available to the public. Here are a few reasons why you might consider participating:
While clinical trials offer many benefits, it’s essential to consider all aspects before deciding to join. Here are some important points to keep in mind:
If you’re interested in participating, talk to your doctor about clinical trials in your area, particularly those focused on PBC or PSC. The United States has several public health databases where you can find trials, including the National Institutes of Health (NIH) and clinical trial listings on hospital and research center websites. You can also go directly and sign up for Science 37 clinical trials. Science 37 offers decentralized clinical trials that allow you to participate from the comfort of your home.
Clinical trials are pushing the boundaries of what’s possible for liver diseases like PBC and PSC. With new studies focusing on slowing liver fibrosis, managing symptoms, and exploring novel immune responses, the current research will likely shape tomorrow’s treatment options. Some trials even aim to address complications like liver cancer, making them critical for long-term liver health.


