
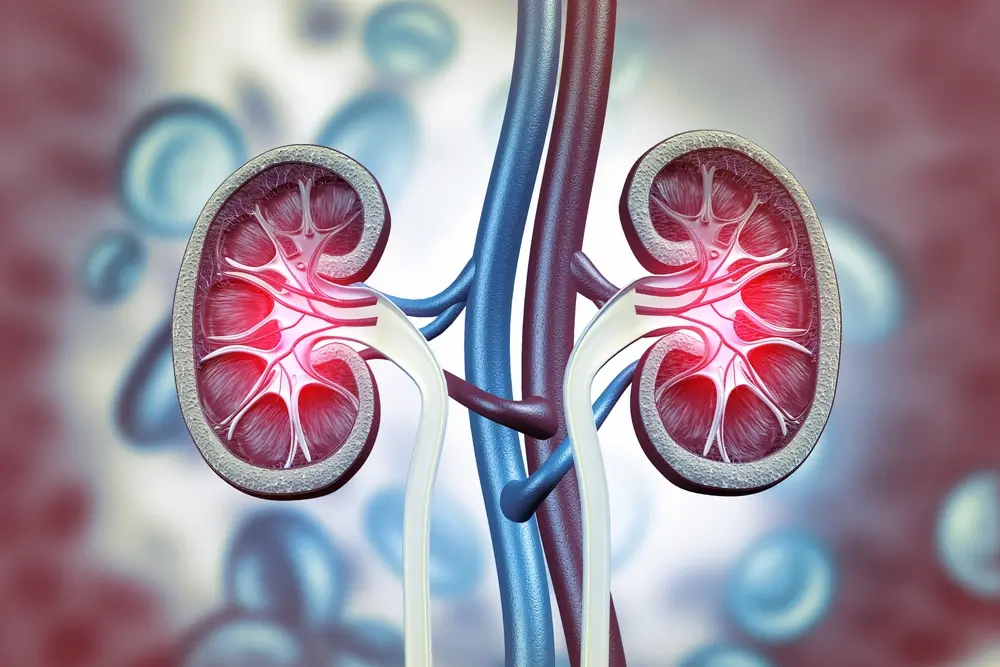
IgA nephropathy, also called Berger’s disease, happens when a protein called immunoglobulin A (IgA) that helps the body fight infections builds up in the kidneys. This buildup causes inflammation and can eventually affect the kidney’s ability to properly filter waste from your blood.
Many people with IgA nephropathy might not realize they have it because it usually doesn’t cause symptoms in the early stages. It can take ten years or more before signs show up, so it’s often called a silent disease.
While there is no cure for IgA nephropathy, there are medications that can help manage the symptoms and sometimes even put the disease into remission.
The disease may not show any symptoms for at least ten years. When symptoms appear, they may include:
If there’s acute kidney failure, these symptoms may appear:
IgA is a protein known as an antibody that helps fight infections. IgA nephropathy happens when too much of this protein builds up in the kidneys. This buildup occurs in the tiny blood vessels in the kidneys, called glomeruli, causing them to become inflamed.
Scientists still do not know exactly why IgA accumulates in the kidneys. However, certain factors can make it more likely to develop this condition:
Family history: In over 10% of cases, IgA nephropathy runs in families, meaning it can be inherited. People who inherit the gene may not show symptoms but could still pass it on
Diagnosis helps rule out other conditions like IgA vasculitis, which also cause symptoms like blood in the urine. There are several methods to test for IgA nephropathy:
Estimated Glomerular Filtration Rate (eGFR): Blood tests assess how well the kidneys can remove waste from the blood
Currently, there is no cure for IgA nephropathy, and it can be challenging to predict how the condition will affect kidney health in the long term.
Some people only need regular medical tests to monitor the progression of the disease, while others may require medication to control symptoms and prevent the condition from worsening.
Various types of medicines can be used to treat IgA nephropathy. These include:
Also known as immunosuppressants, these strong medicines can lower the body’s defenses. They work by preventing the immune system from producing the proteins that affect the glomeruli.
However, these medicines can have potential side effects, including high blood sugar, high blood pressure, and a higher risk of infections. It’s important to work with a healthcare provider to choose the right immunosuppressant.
Medications like angiotensin receptor blockers (ARBs) and angiotensin-converting enzyme (ACE) inhibitors are commonly used to lower blood pressure. By doing so, they also help reduce protein loss in the urine.
Omega-3 fatty acids, common in fish oil supplements, can help reduce inflammation in the glomeruli with fewer side effects. It’s best to seek a doctor’s guidance when choosing prescription supplements.
Diuretics are medicines that help kidneys remove more salt and water from the body through urine. They can also help control edema- swelling in the feet or hands due to fluid buildup.
People with kidney damage are vulnerable to a heart attack or stroke. Controlling cholesterol with medicines, such as statins, can lower this risk.
When there’s kidney failure, it means 85 to 90 percent of kidney function is lost, and dialysis becomes necessary to remove fluids and wastes from the body.
Dialysis helps manage blood pressure by filtering fluids and wastes from the blood. It can be done using a machine (hemodialysis) or a cleansing solution around the belly lining (peritoneal dialysis).
This treatment is a long-term approach to kidney failure and can save patients from needing dialysis multiple times a week. Studies show that people who opt for a kidney transplant live longer than those who use dialysis.
Discussing this option with a doctor is important to determine the best action.

IgA nephropathy progresses differently for each person, depending on overall health and how well the symptoms are managed.
Some people don’t show symptoms and might not even know they have the disease. Others may have symptoms like blood in the urine but still have properly functioning kidneys. Kidney failure can sometimes occur after a few months or several years.
Effective medication can put the disease into remission, meaning the symptoms no longer appear. However, once the kidney is damaged, about one in four people with IgA nephropathy may experience kidney failure. Others might go into remission or continue to have blood or protein in their urine without serious kidney damage.
If diagnosed with IgA nephropathy, the following strategies can help control its symptoms:
Living with IgA nephropathy can be challenging, especially after kidney failure. Fortunately, various treatment options and lifestyle adjustments can help manage symptoms. Additionally, medical research is ongoing to discover more effective treatments for those with the disease.
One promising development is sparsentan, an FDA-approved drug that doesn’t suppress the immune system. More clinical trials are underway, with organizations like Science 37 leading the research. These trials aim to find new treatment options to reduce IgA buildup in the kidneys and alleviate associated symptoms.


