
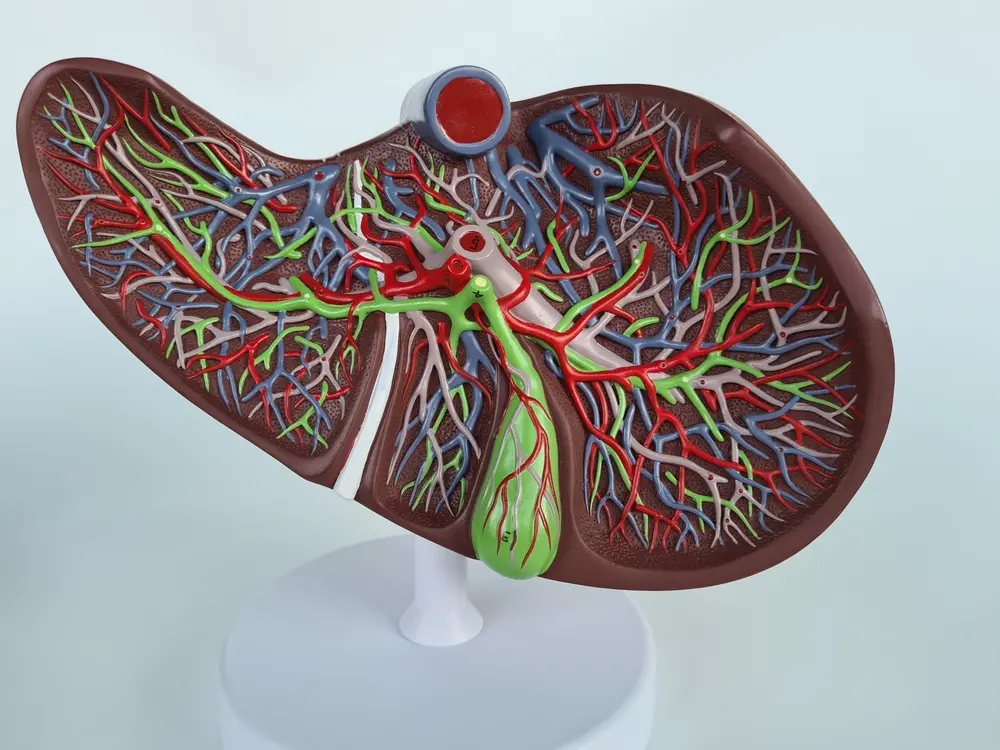
Your liver is an essential organ that performs many crucial functions to keep your body healthy. It processes nutrients from your food, detoxifies harmful substances, produces bile to aid digestion, and helps with blood clotting. Essentially, the liver keeps your body's metabolism running smoothly.
But conditions like primary biliary cirrhosis (PBC) and primary sclerosing cholangitis (PSC) disrupt these functions. Each condition has its unique features and progresses differently, but both may eventually lead to cirrhosis and liver failure. In this guide, we’ll explore how PBC and PSC affect liver function and the mechanisms by which they damage the bile ducts and liver cells.
PBC or primary biliary cholangitis is an autoimmune disease that primarily affects the bile ducts within the liver. So basically, your immune system mistakenly attacks the bile ducts, leading to inflammation and scarring. Over time, this degrades the ducts and makes it harder for bile to flow to your small intestine.
As a result, bile backs up inside your liver and damages the tissue. Scar tissue slowly replaces healthy tissue, and your liver eventually loses its functionality. PBC is chronic and progressive, meaning it doesn’t go away and worsens over time.
PBC progresses slowly through several stages. In the beginning, it’s mild, and you might miss it. But in the end, the liver becomes increasingly scarred, leading to a condition known as cirrhosis. Cirrhosis marks the end-stage of liver disease, where liver function is significantly impaired. If left untreated, this can eventually cause liver failure, which is life-threatening.
The progression of PBC varies from person to person, but understanding its impact is essential for managing the disease. Primary Biliary Cirrhosis symptoms include itching, dry eyes and mouth, and jaundice.

PSC is another chronic liver disease that affects the bile ducts. However, PSC tends to cause inflammation and scarring in both the small and large bile ducts inside and outside the liver. This differs from PBC, which primarily affects the smaller bile ducts within the liver.
The exact cause of PSC is not well understood, but it's believed to be linked to genetic and environmental factors. Like PBC, PSC is also considered an autoimmune disease. It’s worth noting that PSC often accompanies inflammatory bowel disease, particularly ulcerative colitis, hinting at a complex relationship between the liver and immune system.
In PSC, the inflammation causes scarring and narrowing of the bile ducts. This blockage impedes bile flow, leading to liver cell damage. The obstruction of bile acids results in liver inflammation, contributing to the progression of liver disease.
The disease progresses slowly in most people with PSC and causes symptoms like fatigue, abdominal pain, itchy skin, and jaundice. Eventually, you may experience repeated infections, portal hypertension, metabolic diseases, tumors, or liver or duct and liver failure. At the moment, the only known cure for advanced PSC is a liver transplant. However, the disease may recur in the transplanted liver in a small number of patients.
Bile acids play a vital role in digestion, helping to break down fats and absorb fat-soluble vitamins. In both PBC and PSC, the inflammation and scarring of bile ducts can obstruct bile flow, causing bile acids to accumulate in the liver and bloodstream.
This buildup can be toxic to liver cells and contributes to liver disease progression. It can also lead to digestive issues, affecting your body's ability to process nutrients effectively. When bile flow is impaired, it can also impact the small intestine, leading to nutritional deficiencies and digestive discomfort. This disruption in digestion highlights the importance of maintaining healthy bile flow for overall health.
PSC and PBC are both chronic liver diseases that primarily affect the bile ducts. Both diseases are progressive and are thought to have an autoimmune component, where the body’s immune system mistakenly attacks the bile ducts. The attack causes inflammation and subsequent damage. PBC and PSC also cause similar symptoms and side effects like:
But the two are also different in the following ways:
PBC primarily affects the intrahepatic (or small) bile ducts within the liver. In contrast, PSC affects both the intrahepatic (inside the liver) and extrahepatic (outside the liver) bile ducts. While you can treat PBC with medications, PSC is more complicated and has no effective treatment.
PBC is more common in middle-aged women, with about 90%of cases occurring in females. This suggests a potential hormonal or genetic link in its development. On the other hand, PSC tends to affect young to middle-aged men more frequently, although it can occur in both genders.
PBC is not typically associated with other diseases, although some patients may have other autoimmune conditions, such as rheumatoid arthritis or Sjögren's syndrome. PSC, however, has a strong link with inflammatory bowel disease (IBD), particularly ulcerative colitis or Crohn’s disease. Up to 80% of PSC patients may have IBD.
PBC is often diagnosed through blood tests that detect specific antibodies, such as anti-mitochondrial antibodies (AMA) or anti-nuclear antibodies (ANA). These antibodies are present in about 95% of PBC patients and provide a clear marker for diagnosis, making it easier for doctors to identify PBC early.
There are no specific antibodies in PSC like in PBC, making diagnosis more challenging. Instead, PSC is typically diagnosed through imaging studies like MRCP (magnetic resonance cholangiopancreatography) or ERCP (endoscopic retrograde cholangiopancreatography) that reveal characteristic bile duct changes. Liver biopsy may also be used to assess the extent of liver damage.
PBC treatment mainly focuses on managing signs and symptoms and slowing disease progression with medications like ursodeoxycholic acid (UDCA), which helps improve bile flow and reduce liver inflammation. Newer medications are also being explored to offer more targeted therapies for PBC patients.
PSC lacks a specific medical treatment. Treatment often involves managing complications and considering liver transplantation for advanced cases. Endoscopic procedures may be used to manage bile duct strictures, but long-term management still remains a challenge.
Organizations like Science 37 are running trials for new treatments or improving existing ones. If you need more detailed information on clinical trials or specific aspects of treatment, please feel free to ask.


