AFib & Stroke: Uncovering the Risks & Essential Prevention Tips
Atrial Fibrillation (AFib or AF) is a common heart rhythm disorder that affects about 6 million Americans a year. Despite being a heart problem, it also affects the brain. According to studies, people with untreated AF are 5 times more likely to have a stroke than people without AFib. That’s why it’s crucial to understand the connection between AFib and stroke and how to seek help.
Understanding Atrial Fibrillation
Atrial fibrillation (AFib) is a type of irregular heart rhythm where the upper chambers of the heart (the atria) beats out of sync with the lower chambers. Instead of the steady, normal rhythm your heart usually follows, AFib causes it to beat rapidly and unevenly. This irregular heartbeat can feel like a fluttering or pounding sensation in your chest. Some people with AFib don’t even notice the symptoms, while others might experience dizziness, shortness of breath, or fatigue.
AFib becomes more common as we age, but it can affect people at any stage of life. Along with common risk factors like high blood pressure, heart failure, and obesity, lifestyle habits like smoking and drinking alcohol excessively can increase your chances of developing AFib. Living with AFib means your heart isn’t pumping blood as efficiently as it should, which is where the risk of stroke comes in.
The Link Between AFib and Stroke
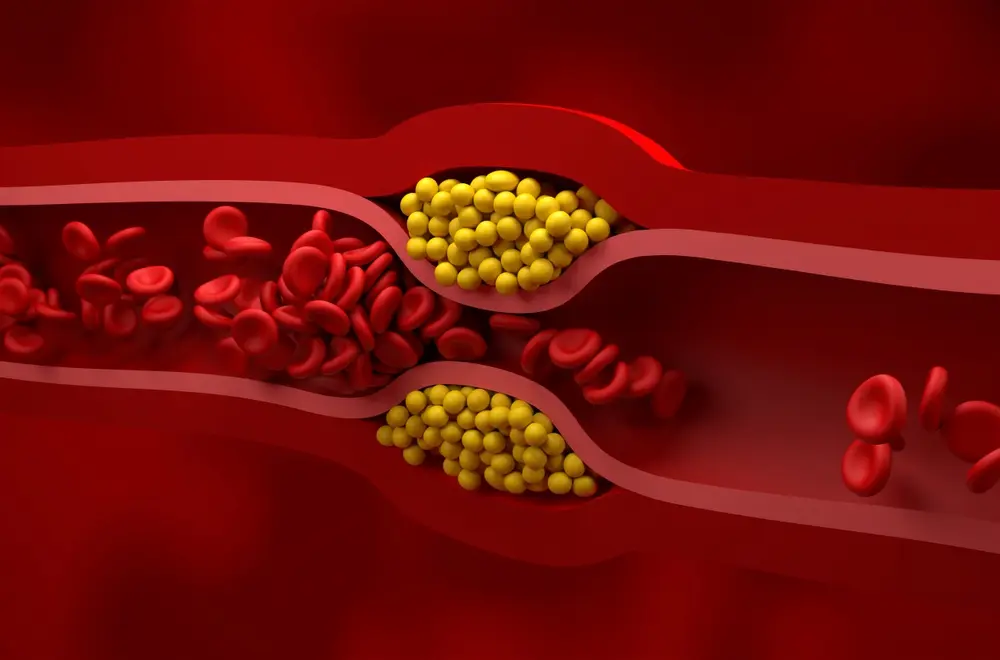
When your heart is in AFib, the upper chambers, or atria, do not beat effectively. Instead of pumping blood normally, the atria quiver or flutter. This irregularity means blood can pool in these chambers, especially in a small pouch known as the left atrial appendage. When blood remains stagnant, there’s a higher chance for blood clots to form.

If a blood clot dislodges and enters the bloodstream, it can travel to the brain, blocking a vital artery. This blockage cuts off the oxygen supply to part of the brain, causing a stroke. Strokes damage brain cells, leading to permanent loss of function and affecting speech, movement, and cognitive abilities.
Beyond that, many people with AFib also have high blood pressure, which is another significant risk factor for stroke. High blood pressure puts extra strain on the heart and blood vessels, making strokes more likely. AFib is also linked to other heart problems like heart failure and coronary artery disease, which further increase stroke risk. When your heart is already under stress from other conditions, AFib can push it to a breaking point.
How Much More at Risk Are You?
People with untreated AFib are more likely to suffer a stroke than those without it. Studies show that nearly 1 in 7 strokes are linked to AFib. This means it’s not just a heart issue—it’s a major risk to your brain health, too. In fact, strokes caused by AFib tend to be more severe and have worse outcomes than other types of stroke because the clots formed in the heart tend to be larger.
The irregular heart rhythm in AFib disrupts the smooth flow of blood through the heart, making it easier for clots to form. The longer AFib goes untreated, the greater the risk of a stroke.
Recognizing the Early Warning Signs of Stroke

If you have AFib, it’s important to recognize the early signs of a stroke. Acting quickly can save your life and prevent long-term damage to your brain cells. Remember the acronym FAST:
- Face: Is one side of your face drooping?
- Arms: Can you raise both arms or is one weaker?
- Speech: Is your speech slurred or hard to understand?
- Time: If you notice any of these symptoms, it’s time to call 911 right away.
The faster you receive medical attention, the better your chances of recovery.
The Importance of Regular Checkups

If you’re living with atrial fibrillation AFib, schedule regular checkups with your healthcare provider to help you keep your condition in check. Your doctor will monitor your heart rate, adjust medications, and check for other risk factors like high blood pressure or heart failure. Early detection of changes in your heart rhythm or overall health can significantly prevent a stroke.
Exploring Clinical Trials and Research Studies
Although there is currently no cure for AF, clinical trials and research studies are always underway to test new therapies. If you’re interested, learn more about participating in a clinical trial with Science 37. You may contribute to research that could help others in the future.