
About 795,000 people in the US suffer stroke every year. According to new reports, someone gets a stroke every 40 seconds, and every 4 minutes, someone dies from a stroke. It’s heartbreaking to think about, especially knowing that strokes don’t just take lives—they can also lead to long-term severe disabilities.
Of the 7 million stroke survivors, two-thirds are disabled, and 25% will have another stroke within just five years. But the good news is up to 80% of strokes may be preventable with exercise, better nutrition, and identification of risk factors.
Strokes occur when the brain’s blood supply is interrupted, either by a blockage or a rupture in a blood vessel. Atrial fibrillation (AFib) is a considerable risk factor for stroke. When you have AFib, the upper chambers of the heart beat irregularly and out of sync with the lower chambers. Irregular heartbeats (heart arrhythmia) can cause blood to pool and form clots in your heart. If a clot escapes and travels to your brain, it can block blood flow and cause a stroke.
Currently, there’s no known cure for AFib. But there’s treatment to help control symptoms and prevent complications. Researchers are continuously exploring new ways to treat atrial fibrillation and prevent stroke. Let’s explore some innovative stroke prevention strategies.
Novel anticoagulants, also called direct oral anticoagulants (DOACs), are a newer and often preferred option for many patients. These medications target specific clotting factors in your blood to prevent clots from forming.
Here are the most common DOACs prescribed for a range of heart diseases, including cardiac arrhythmia:

Warfarin has been used for decades. But it's among the top 10 drugs with the highest number of serious side effects reports submitted to the US FDA during the last 20 years. The biggest safety concern of this drug is the risk of major bleeding.
Warfarin also requires frequent blood tests and comes with dietary restrictions because it interacts with foods high in vitamin K. DOACs, on the other hand, offer similar anticoagulation benefits but with fewer complications.
DOACs are often recommended for AFib patients who need anticoagulants, especially if you’re at risk of stroke but don’t want the hassle of constant monitoring. However, they may not be suitable if you have certain conditions, like severe kidney disease.
If you’re currently on warfarin or haven’t started anticoagulation therapy, talk to your doctor about whether a DOAC could be a better option for you. These medications are helping countless people with AFib live safer, more manageable lives.
For some patients with atrial fibrillation (AFib), long-term use of blood thinners isn’t an ideal option due to risks like excessive bleeding or other medical conditions. In these cases, left atrial appendage (LAA) closure devices offer an alternative way to reduce the risk of stroke. These devices block the LAA, a small pouch in the upper chamber of the heart where blood clots often form in AFib patients, preventing clots from getting into the bloodstream and causing a stroke.
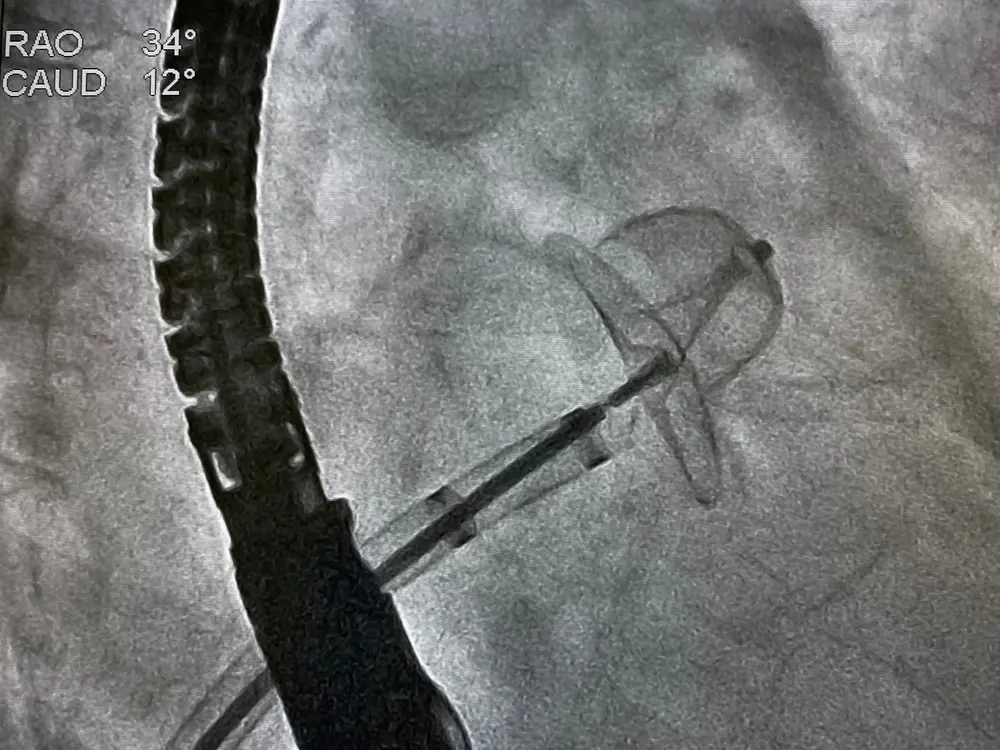
These devices are implanted in the heart to seal off the LAA and stop blood from pooling and clotting in this area. Several LAA closure devices are currently available, each with unique features:
Implanting an LAA closure device is a minimally invasive procedure. Here’s what you can expect:
Innovative treatments like the ablation procedure, LAA, and DOACs have revolutionized stroke prevention for people with AFib. They significantly lower stroke risk and improve quality of life, but they don’t cure AFib. That’s why clinical trials are still essential.
AFib is a complex condition with persistent and long-standing impacts on heart rhythm and overall health. Current treatments aim to control symptoms, reduce the risk of stroke, and improve daily life, but a true cure remains elusive. Clinical trials focus on addressing these gaps by:
Participating in a trial gives you access to new treatments that may not be available yet at your local medical center. It also helps researchers gather essential data to improve care for people living with AFib.
If you want to join a clinical trial, talk to your healthcare provider first. They can help you determine if you qualify based on factors like age, medical history, and the type of AFib you have (persistent or long-standing).
Many trials are looking for participants who have specific symptoms, like chest pain or heart failure, or those who are struggling to manage their risk of stroke. When you participate in a clinical trial, you’re not just helping yourself—you’re helping others by advancing medical science. Many participants report feeling empowered by their role in shaping the future of healthcare.If interested, speak with your doctor or contact a medical center conducting AFib trials to learn about your options. You can also enroll to participate in Science 37’s pioneering research for heart and blood disorders.


