
Sepsis is one of the leading killers in the United States, and it often slips by unnoticed until it’s too late. You won’t see it plastered on billboards like heart disease, and it doesn’t get the kind of media coverage that cancer does. Yet the numbers are staggering.
Each year, around 1.7 million people are diagnosed with sepsis, and nearly 350,000 die from it. That’s one out of every three hospital deaths. Think about that for a second. Every 90 seconds, someone loses their life to sepsis. Even more sobering, it takes the lives of more children each year than cancer.
What’s scary is that most people have no idea what sepsis even is until it strikes someone they love. It doesn’t announce itself with a clear label. It can start as something small, a cut that looks irritated, a urinary tract infection that lingers, or a cough that won’t go away, and then, suddenly, the body’s response spirals out of control. A seemingly minor infection can turn into a full-blown medical emergency before you even realize what’s happening.
That’s why Sepsis Awareness Month exists. This is the time to pull back the curtain on a condition that has touched countless families but remains misunderstood. The more we talk about it, the more people recognize the signs and symptoms of sepsis, and the faster they can act. Awareness truly is the first step toward saving lives.
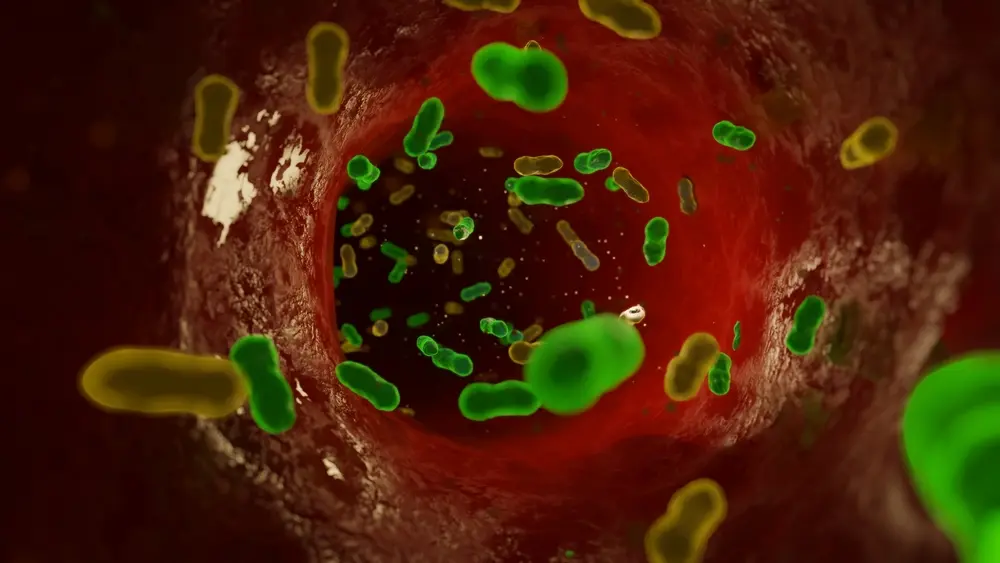
At its core, sepsis happens when the body’s response to an infection goes haywire. Normally, when a bacterial infection sets in, the immune system releases white blood cells to fight off the invader. That’s how healing usually works. But sometimes, the immune system goes into overdrive. Instead of helping, the response floods the body with chemicals that trigger massive inflammation.
This causes damage to tissues and vital organs like the lungs, heart, or kidneys. When the body can’t keep up, things spiral quickly toward organ damage and, in the most dangerous cases, septic shock, where blood pressure crashes.
Sepsis isn’t just a bad infection. It’s the body turning against itself, and it can become fatal in hours. That’s why healthcare professionals stress that sepsis is always a medical emergency.
The frightening thing about sepsis is how fast it moves. Someone might feel fine in the morning, only to fight for their life by evening. The faster sepsis is recognized, the higher the chance of survival.
A helpful tool to remember is the “It’s About TIME” campaign:
Every one of these red flags points to danger. If you notice them, don’t wait and see if things improve. Call for help, head to the ER, and make sure the doctors check for sepsis.
Sepsis can strike anyone, but some groups are especially vulnerable:
That said, don’t think sepsis only happens to “other people.” Healthy, active adults can develop it too. A skin wound, a dental abscess, or even the flu can be enough to set it off.
Spotting sepsis early means knowing what to look for. Common signs and symptoms of sepsis include:
When an infection advances to sepsis and septic shock, blood pressure plummets, organs fail, and death can come quickly without treatment.
Doctors diagnose sepsis by checking vital signs, running blood tests, and confirming the presence of infection. Quick action with IV antibiotics, fluids, and supportive care is the only way to turn things around.
Sepsis is the third most common cause of death in US hospitals. Beyond the immediate danger, survivors often face long-term complications. Recovery can be grueling, with problems like:
This is sometimes called post-sepsis syndrome. It affects patients physically and mentally. Families often describe it as a complete shift in their loved one’s life, sometimes making it difficult to return to work or manage daily activities.

The truth is, you can’t prevent every case of sepsis, but you can reduce the odds. Here’s what helps:
Ever wonder why September spotlights sepsis? It’s because awareness truly saves lives. During Sepsis Awareness Month, families, survivors, and organizations flood social media with resources, personal stories, and a powerful reminder: sepsis isn’t rare.
Talking about it openly makes all the difference. The more people who know the warning signs, the faster they can act when it matters most. Even something as simple as sharing a post online might help someone recognize the danger in time, and that could be the very thing that saves their life.
Sepsis has been a puzzle for researchers for decades. Because it develops quickly and varies so much from patient to patient, running clinical trials for sepsis has always been complicated. Still, progress is being made.
Scientists are working on faster ways to diagnose sepsis, stronger drugs to fight bacterial infections, and treatments to limit organ damage. Some trials focus on helping the immune system respond more effectively instead of spiraling out of control.
One of the most promising changes is the growth of decentralized clinical trials. Instead of patients needing to travel to big hospitals for every visit, these trials can often be done closer to home, through local clinics, telehealth, or even wearable devices that track vital signs. This makes it easier for more people to take part, which speeds up discoveries and brings us closer to better treatments.
Science 37 is leading the way in this shift, making it possible for patients and families to contribute to research without leaving their communities. It’s a step toward more hope, more answers, and ultimately, more lives saved.


